A new study from The American Journal of Managed Care highlights the limitations of traditional patient portals – and points the way toward a more accessible future.
Digital health has the power to transform patient outcomes, but only if patients actually use the tools provided. For years, the healthcare industry has relied on the “Patient Portal” as the gold standard for digital engagement. However, a startling new study published in the January 2026 issue of The American Journal of Managed Care (AJMC) reveals that for many vulnerable populations, the portal is not a bridge to care – it is a barrier.
The study, titled “Insights Into Patient Portal Engagement Leveraging Observational Electronic Health Data,” analyzed over 250,000 adults with chronic conditions. The findings offer a critical wake-up call for health systems relying solely on portal-based strategies.
The Reality Check: What the Data Says
The researchers looked at a massive dataset of patients aged 50 and older managing chronic conditions like diabetes, hypertension, and heart failure. While the clinical need for engagement was high, the actual digital adoption was telling:
- Activation vs. Usage: While 61% of patients went through the trouble of activating their portal accounts, only 54% actually logged in for at least one session.
- The Age Gap: Engagement dropped significantly for patients over the age of 65 – the very demographic that often requires the most frequent care.
- The Equity Gap: The study found glaring disparities. Portal usage was significantly lower among Black patients and non-English speakers (specifically Somali, Spanish, and Hmong speakers).
- The Education Gap: Patients with less than a college degree were far less likely to utilize the portal.
The authors of the study concluded that “tool-related barriers” and “digital health equity gaps” are preventing optimal care. They explicitly called for “multilingual, literacy-appropriate strategies” to expand access.
Why Portals Are Struggling
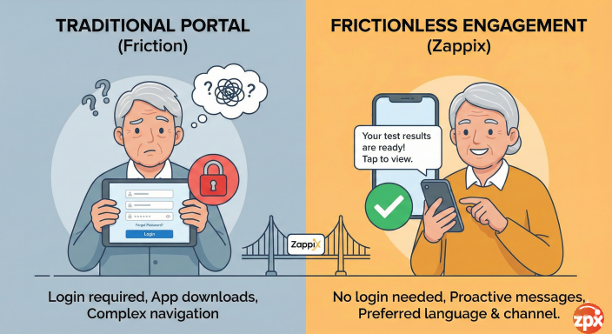
The AJMC study underscores a fundamental flaw in the traditional engagement model: friction.
Portals require patients to download apps, remember complex passwords, navigate dense interfaces, and proactively seek out information. For an older adult, a non-native English speaker, or someone with limited digital literacy, these are not small hurdles – they are walls.
When healthcare providers rely exclusively on portals, they inadvertently leave behind the patients who need support the most.
The Zappix Advantage: Engagement Without Barriers
The data is clear: to reach 100% of the patient population, we must move beyond the “login wall.” This is where Zappix changes the paradigm.
Zappix addresses the exact disparities highlighted in the AJMC study by removing the friction from digital health. Instead of waiting for patients to log in, Zappix proactively reaches out to them.
Here is how Zappix solves the challenges identified in the study:
1. No Logins, No Downloads, No Friction
The study cited “tool-related barriers” as a major hurdle. Zappix eliminates this entirely. Our Digital Patient Engagement solution utilizes frictionless web-apps. There is no app to download and, crucially, no login required. Patients simply click a secure link and have immediate access to the tools they need. By removing the password barrier, we open the door for the older and less tech-savvy populations that portals leave behind.
2. Meeting Patients Where They Are
The study showed that passive availability isn’t enough. Zappix engages patients using their preferred contact method, whether that is text (SMS) or email. We send the exact information they need, exactly at the right time. whether it is a pre-procedure checklist, a post-discharge instruction, or a chronic care check-in. This proactive approach ensures high engagement rates without requiring the patient to be the initiator.
3. Bridging the Language & Literacy Gap
The AJMC findings on non-English speakers are concerning. If a patient cannot understand their instructions, outcomes suffer. Zappix engages patients in their preferred language. Our platform automatically adapts to the patient’s needs, ensuring that language is never a barrier to care. Furthermore, our visual, easy-to-navigate interfaces are designed for accessibility, catering to varying levels of digital literacy.
Conclusion
The AJMC study is a valuable reminder that “access” to technology is not the same as “engagement” with it. As long as we hide critical health information behind login screens and complex portals, the digital divide will persist.
At Zappix, we believe that digital health should be effortless. By leveraging frictionless, proactive, and accessible technology, we can turn the insights from this study into action, ensuring that every patient, regardless of age, background, or language, stays connected to their care.